IN APPEALING IMPROPER DENIALS, FINDING THE RIGHT WORDS CAN BE DIFFICULT.
According to RevCycle Intelligence, “hospitals and health systems could collectively lose $53 billion in revenue in 2021…but that could increase to as much as $122 billion…” Furthermore, “many hospitals will not be able to survive the damage to their cash flow for longer than 60-90 days.”
How much smaller would that statistic be if providers had the right words?
Third-party payors process a huge volume of accounts, delaying and denying payment on thousands of claims every year. They do this knowing that most inconsistent practices are accepted without question and that medical providers do not have the time and legal expertise to write appeal letters.
N O W Y O U D O.
RevAssurance Online commands the knowledge and tools used by the Claims Compliance Experts of ERN/The Reimbursement Advocacy Firm.
| Write More Powerful Appeals | |
| Respond to Problematic Payors with Statutes, Regulations, and Case Law | |
| Reduce Days in Accounts Receivable and Bad Debt Write Offs | |
| File Online complaints with State and Federal Regulatory Agencies | |
| Preserve Patient Access to Care | |
| Educate Patients on their Rights |
At ERN, we strive to provide the industry with the very best education and tools for reimbursement advocacy, and to help you advocate for medically appropriate healthcare pursuant to Wickline vs. State.
RevAssurance Online is also a robust training program for new and existing employees to access administrative laws that enforce timely reimbursement and combats improper denials.
As a member, you will receive early access to all the new resources offered in RevAssurance Online, including:
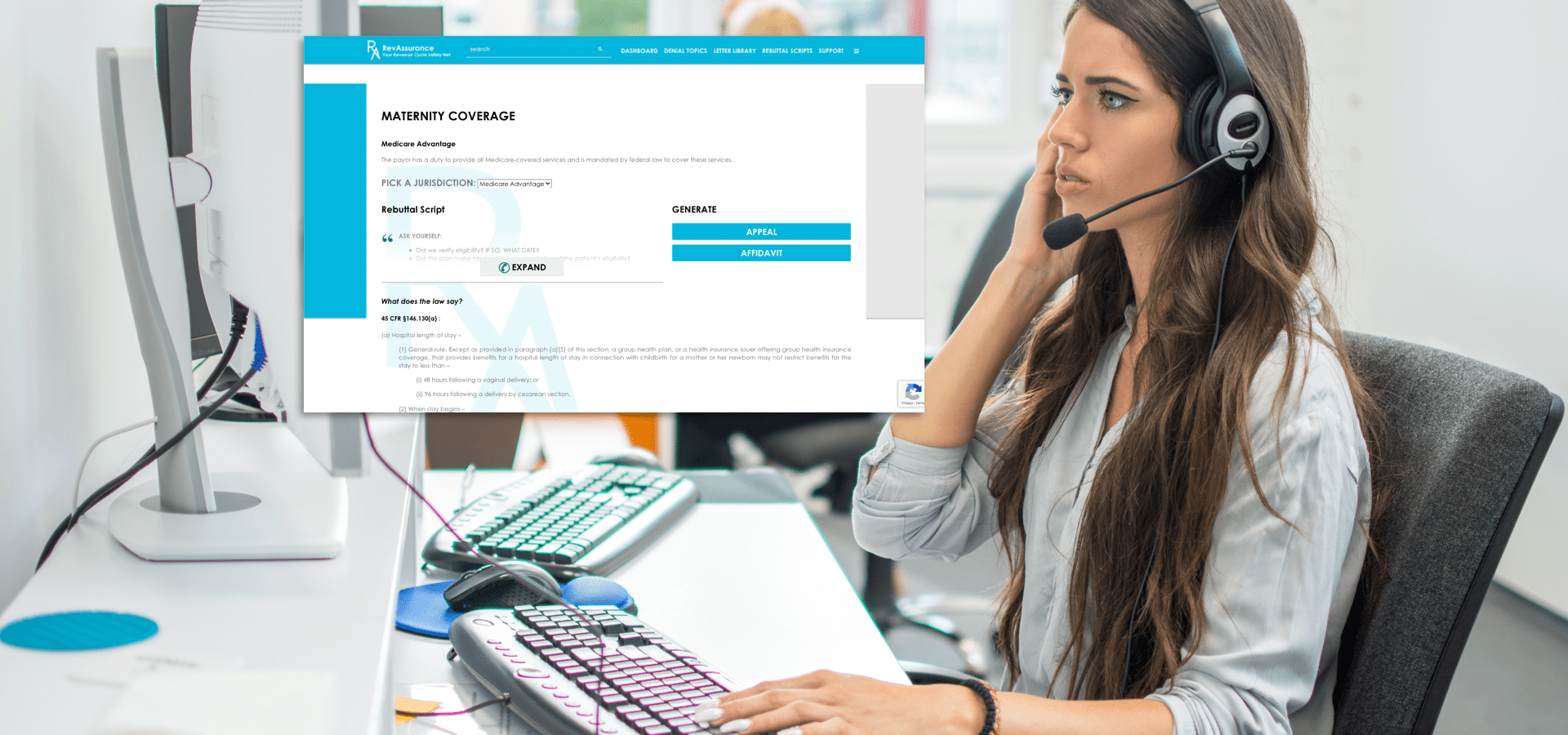
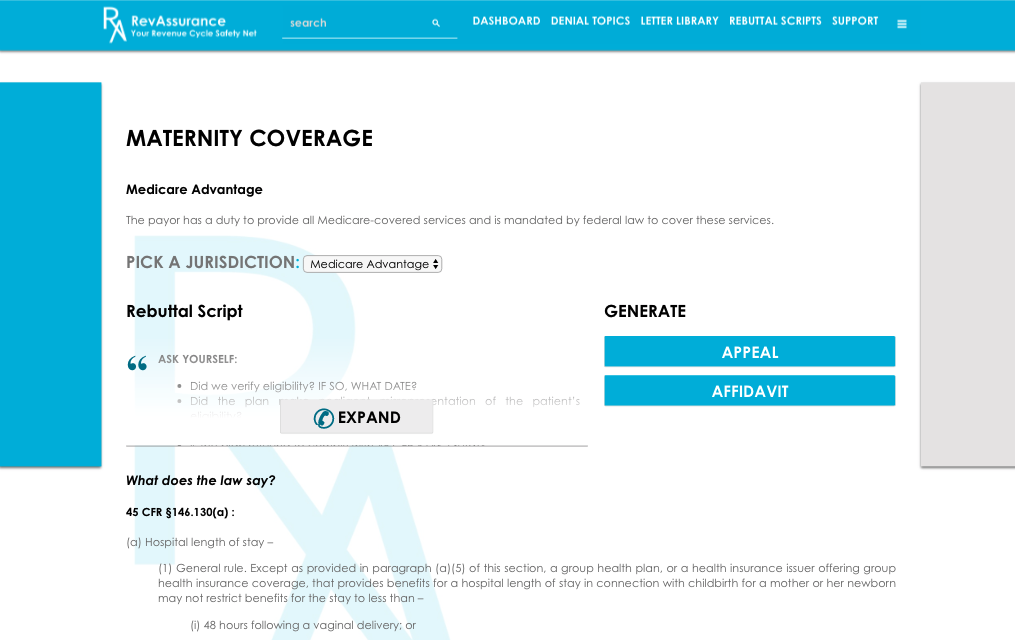
- Denial Topics Encyclopedia
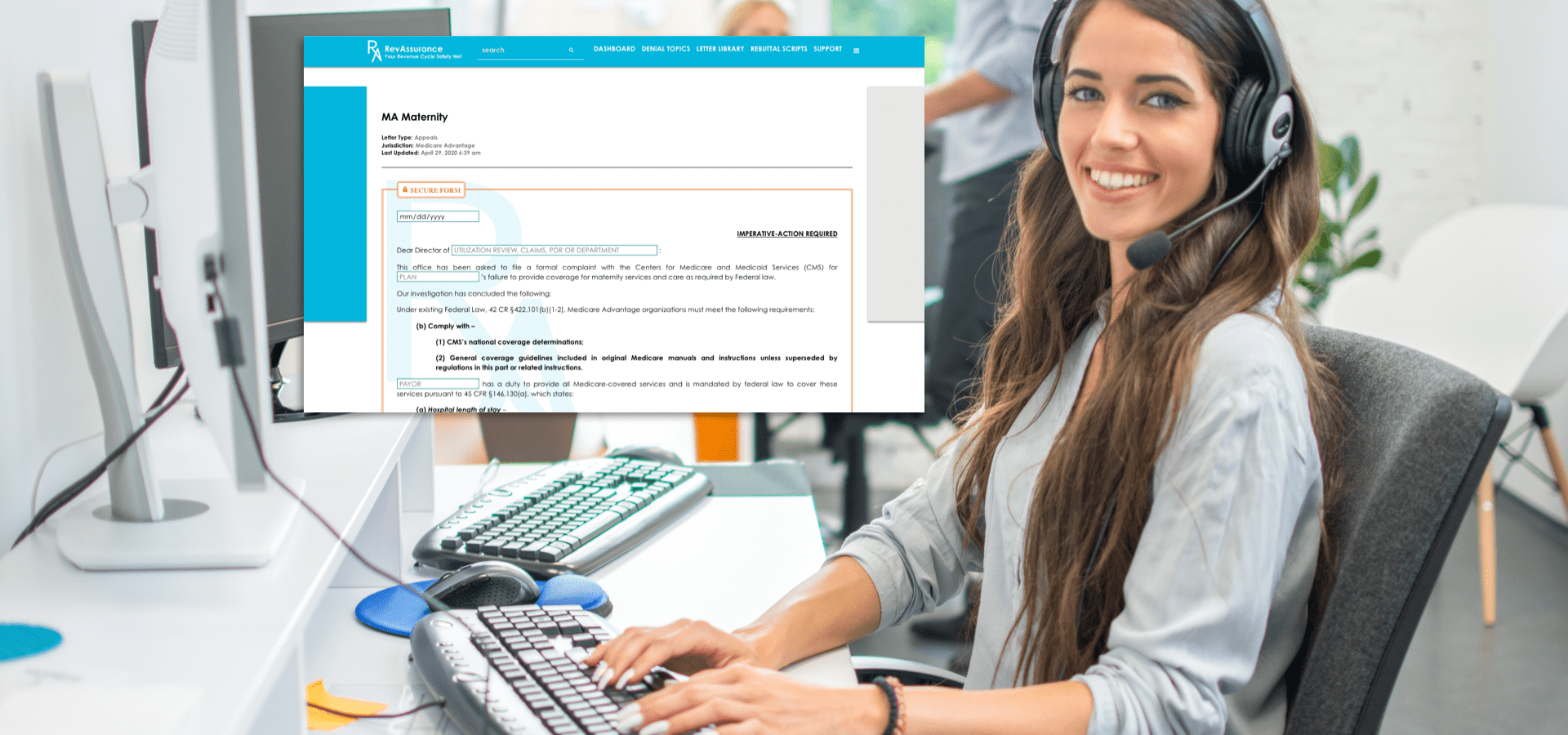
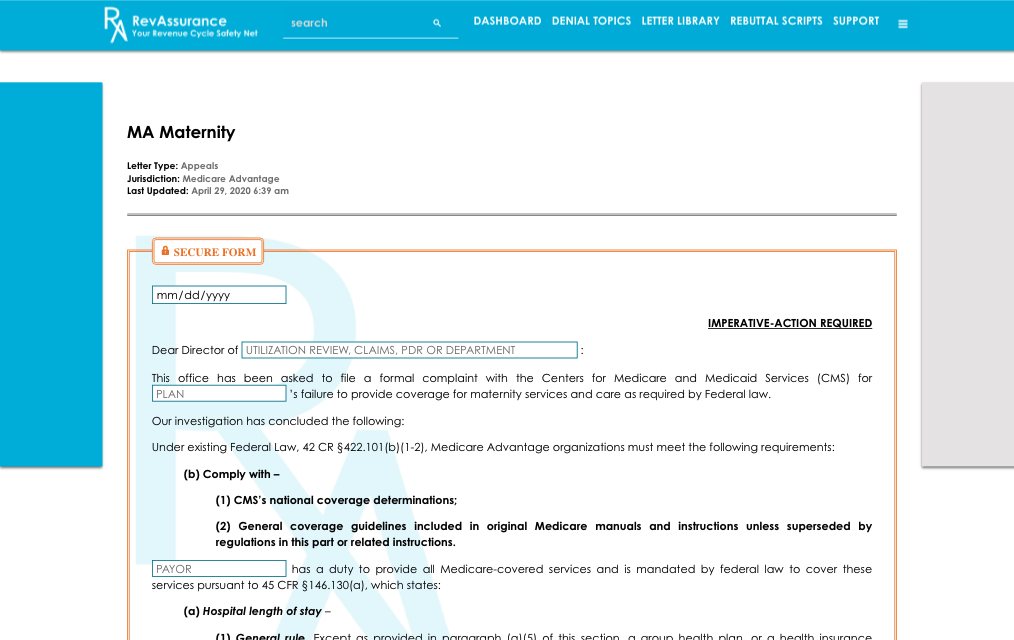
- The New Appeal Letter Generator
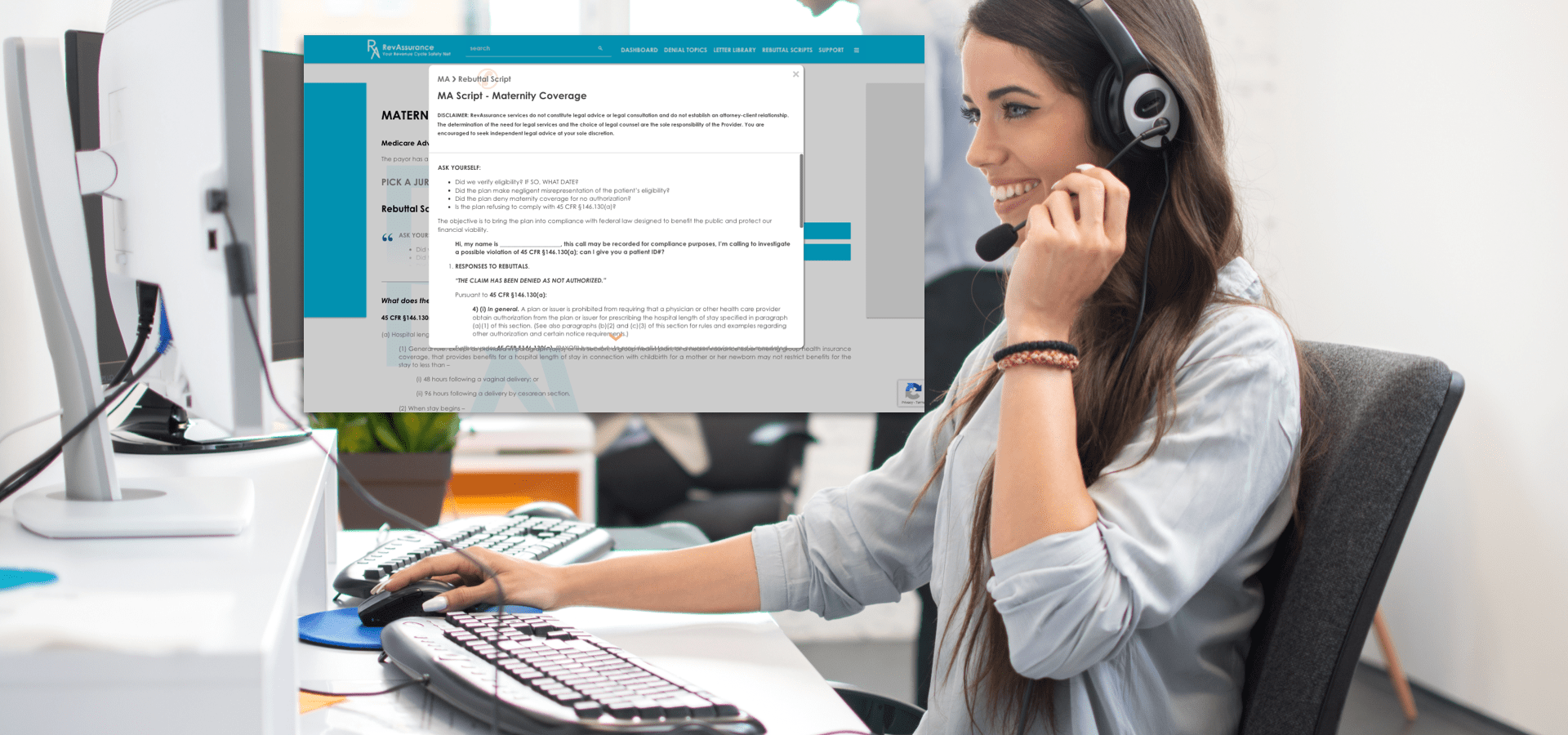
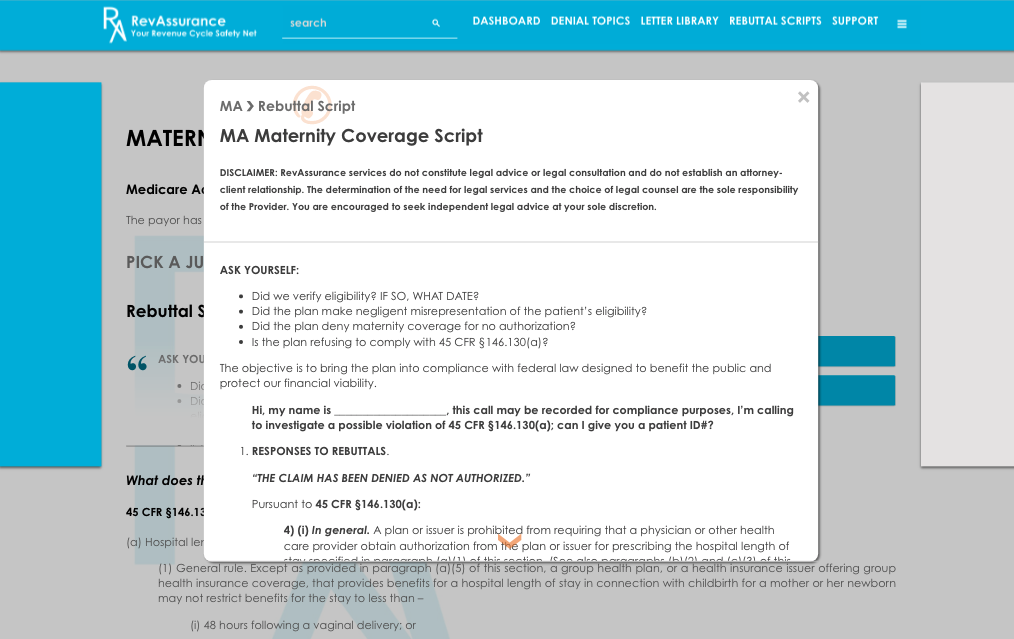
- A Library of Rebuttal Scripts
- A map of Regulatory Agencies and their jurisdictions
- Interest Calculation Resources