MYTHBUSTER: Are MA plans required to respond to inpatient authorization requests?
MYTH: MA Plans are not required to respond to an inpatient authorization request.
FACT: MA Plans ARE required to respond to an inpatient authorization request.
Under 42 CFR §422.113(c)(2)(iii):
(2) MA organization financial responsibility. The MA organization:
(iii) is financially responsible for post-stabilization care services obtained within or outside the MAO that are not pre-approved by a plan provider or other MAO representative, but administered to maintain, improve, or resolve the enrollee’s stabilized condition if –
(A) the MAO does not respond to a request for pre-approval within 1 hour;
(B) the MAO cannot be contacted; or
(C) the MAO representative and the treating physician cannot reach an agreement concerning the enrollee’s care and a plan physician is not available for consultation. IN this situation, the MAO must give the treating physician the opportunity to consult with a plan physician and the treating physician may continue with the care of the patient until a plan physician is reached or one of the criteria in 422.113(c)(3) is met.
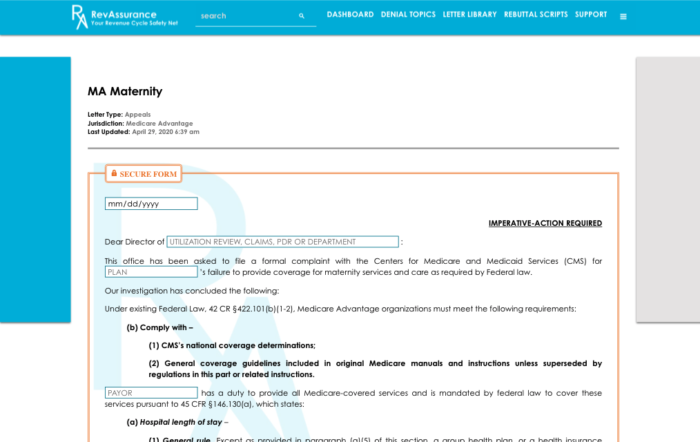
With RevAssurance Online’s letter library, generating an appeal letter to require MA plans to respond to inpatient authorization requests has never been easier! Simply fill in the blank fields and hit “Generate Letter”. The best part about our letter generator? It has the secure form feature so that your letters remain HIPAA compliant! Make sure you’re getting properly reimbursed for services you’ve rendered.
Tags: mythbusters
Categorised in: General
This post was written by RevAssurance

