Obtaining Authorization While Patient Is In House
A large 11 hospital provider member recently submitted a complaint to ERN/TRAF against a health plan who failed to approve or disapprove authorization within one (1) hour of contact being made and denied the claim stating the provider had notified them 23 days after patient admission and instructed the provider to bill the claim with clinical documentation after patient discharge. This would have resulted in an immediate backend denial and delayed revenue capture through the reconsideration process.
Timeline:
- On 09/21/2021, the patient presented to the hospital with an emergent medical condition and was unable to answer questions given the violent and aggressive nature of his behavior.
- On 09/22/2021, the hospital notified the health plan of the patient’s admission and requested inpatient authorization.
- On 10/14/2021, the health plan failed to respond to the hospital’s request for inpatient authorization and the hospital faxed an authorization demand letter citing the health plan’s failure and violation of federal law.
- On 10/15/2021, the health plan finally responded, but then stated notification was made 23 days following the patient’s admission. The health plan failed to take into account the hospital’s notification on 09/22/2021.
- On 11/29/2021, ERN/TRAF reached out to the health plan who noted that they have not reached a determination on issuing authorization or determining placement for this patient after the patient has been in the inpatient level of care for sixty-nine (69) days.
Pursuant to 42 CFR 422.113 (c)(2)(iii):
(2) MA organization financial responsibility. The MA organization:
(iii) is financially responsible for post-stabilization care services obtained within or outside the MAO that are not pre-approved by a plan provider or other MAO representative, but administered to maintain, improve, or resolve the enrollee’s stabilized condition if –
(A) the MAO does not respond to a request for pre-approval within 1 hour;
(B) the MAO cannot be contacted; or
(C) the MAO representative and the treating physician cannot reach an agreement concerning the enrollee’s care and a plan physician is not available for consultation. IN this situation, the MAO must give the treating physician the opportunity to consult with a plan physician and the treating physician may continue with the care of the patient until a plan physician is reached or one of the criteria in 422.113(c)(3) is met.
Pursuant to 42 CFR 422.113 (C)(2)(iii), the health plan is ultimately responsible for the timely reimbursement of this claim as they failed to issue a timely organization determination within (1) hour either approving or disapproving services and assuming care of the patient. Thus, these post-stabilization services were deemed authorized after they failed to authorize or assume care of the patient and arrange for transfer within one (1) hour from the time the emergency provider submitted inpatient authorization requests and clinicals.
In the first sixty-one (61) days the patient was in house, the health plan denied services that were rendered. On 11/29/2021, ERN/TRAF submitted a Summary of Complaint and notified the health plan that the complaint had been sent. On the next day, 11/30/2021, the health plan sent a notification of authorization for all dates of services concurrently as the patient was still hospitalized. With ERN’s help, an authorization was secured in just eight (8) days for all dates of service (11/22/2021-4/22/2022).
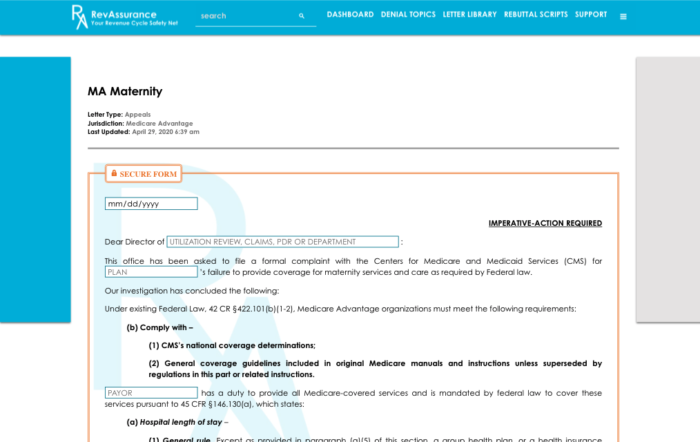
With RevAssurance Online’s letter library, generating an appeal letter to require MA plans to respond to inpatient authorization requests has never been easier! Simply fill in the blank fields and hit “Generate Letter”. The best part about our letter generator? It has the secure form feature so that your letters remain HIPAA compliant! Make sure you’re getting properly reimbursed for services you’ve rendered.
Categorised in: Industry Updates
This post was written by revassurance

