Letter Library
The RevAssurance Letter Library is the flagship feature of the RevAssurance experience. Since 2003, our team has worked to assemble a powerful catalog of sharp templates to defend patient and provider rights.
Each letter in our library is uniquely crafted to address specific categories of claim denials or payment delay tactics. A sampling of our topics include:
- Cease and Desist from conducting retrospective review
- 30 Day Untimely Payment Demand
- 100% Billed Charges Due
- Medical Necessity Appeal
- Authorization for Poststabilization Services and Care
- Disagreement of Care
- Untimely Filing
Further, our letters are tailored address plans from myriad payor jurisdictions. If you purchase a legacy product, such as “REVAssurance 4.5” you will receive letters for such jurisdictions including:
- Medicare Advantage Plans
- Department of Veteran Affairs Fee Basis (non-VA) Care claims
- ERISA Plans
- CA Knox-Keene Licensed Plans
- CA PPO Plans
- Medi-Cal Plans
- Medi-Cal HMOs
- CA Workers Compensation Claims
With RevAssurance Online, we now offer various subscription packages for different jurisdictions. Our base package, RevAssurance Online Federal, includes resources for Federal Jurisdictions including: Medicare Advantage, ERISA, and Veterans Affairs claims. Online Professional, Online Enterprise, and State Components offer even more jurisdictions.
RevAssurance Online, also now provides a brand new Letter Generator. You enter claim details into our forms and RevAssurance will generate and download a Microsoft® Word document.
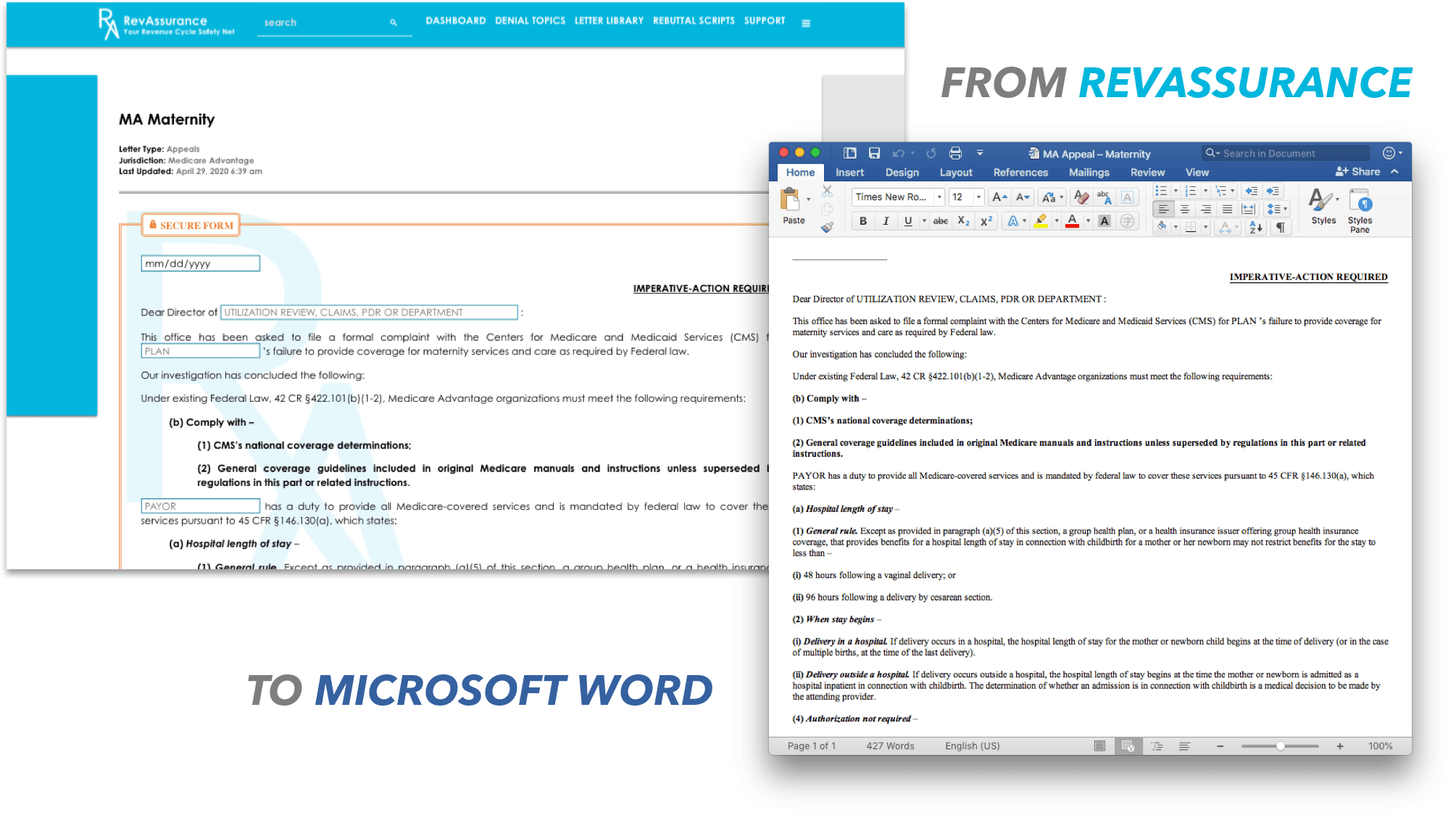
IMPORTANT: Please note that most submission forms on this site are not protected by security mechanisms. Therefore, please refrain from including sensitive information and the unsecured transfer of PHI which could constitute a HIPAA violation. The exception to this rule are areas where you see “SECURE FORM,” on our Letter Library pages. If you see a form guarded by this orange border, feel free to enter PHI and claim details. These forms do not transmit any data across the internet.

